Inside your tooth, under the enamel and a hard layer called dentin, is a soft tissue called dental pulp. This tissue contains blood vessels, nerves, and connective tissues, which help grow the root of your tooth during its development. If the bacteria in the oral environment have reached the dental pulp due to caries, cracks, fractures, it causes pain. Root canal treatment is the process of cleaning, disinfecting, and sealing the pulp tissue in the root canals to get rid of this pain and to prevent re-infection. During root canal treatment, your endodontist:
- Places a dental dam (tiny tarp) over your tooth to isolate the affected area and protect your mouth.
- Accesses the pulp tissue from the top or behind your affected tooth generally by cleaning the tooth decay.
- Removes damaged or diseased pulp tissue.
- Cleans and disinfects the area inside a tooth.
- Fills and seals the tooth.
Endodontists are sometimes called root canal dentists. While general dentists and endodontists can both perform root canal treatment, endodontists perform this procedure much more often. This higher volume and additional training translate to endodontists’ higher level of expertise in performing root canal treatment.
Endodontists specialize in diagnosing complex causes of tooth pain. They also perform other dental treatments, including:
- Endodontic retreatment: Removes and replaces materials used during a previous root canal that did not heal properly.
- Emergency dental surgery: May involve repairing complex dental injuries or treating severe tooth infections.
- Endodontic surgery: Specialized surgery, such as apicoectomy (removal of the end, or tip, of a tooth’s root).
What is endodontics

The term “endodontics” is derived from two Greek words “endo” meaning inside and “odons” meaning tooth.
Taken together, these words mean the branch of dentistry concerned with diseases and injuries of the soft tissues inside a tooth or the dental pulp.
Endodontics come from 2 Greek words, “endo” and “odons” meaning ‘inside tooth’. Endodontics has become the dentistry speciality addressing diseases and injuries of the soft tissue inside a tooth.
What is root canal treatment?
Inside your tooth, under the enamel and a hard layer called dentin, is a soft tissue called dental pulp. This tissue contains blood vessels, nerves and connective tissues, which help grow the root of your tooth during its development. If the bacteria in the oral environment have reached the dental pulp due to caries, cracks, fractures, it causes pain. Root canal treatment is the process of cleaning, disinfecting and sealing the pulp tissue in the root canals to get rid of this pain and to prevent re-infection.
What happens in root canal treatment?
During root canal treatment, your endodontist:
- Places a dental dam (tiny tarp) over your tooth to isolate the affected area and protect your mouth.
- Accesses the pulp tissue from the top or behind your affected tooth generally by cleaning the tooth decay.
- Removes damaged or diseased pulp tissue.
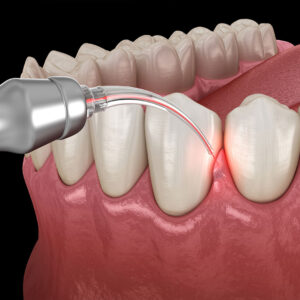
- Cleans and disinfects the area inside a tooth.
- Fills and seals the tooth.



FAQ
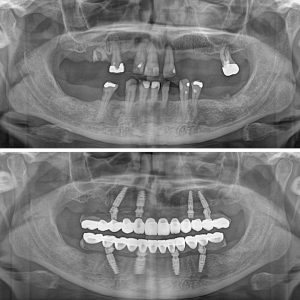
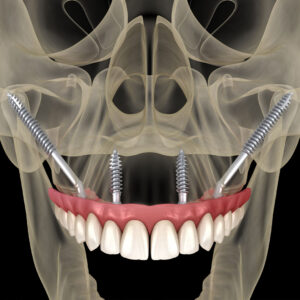
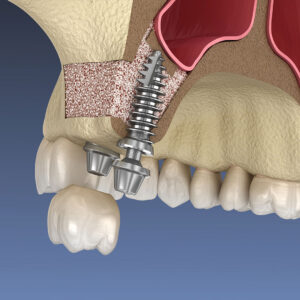
Frequently asked questions about Dental Implants in Turkey
Endodontists are sometimes called root canal dentists. While general dentists and endodontists can both perform root canal treatment, endodontists perform this procedure much more often. This higher volume and additional training translates to endodontists’ higher level of expertise in performing root canal treatment.
Endodontists specialize in diagnosing complex causes of tooth pain. They also perform other dental treatments, including:
- Endodontic retreatment: Removes and replaces materials used during a previous root canal that did not heal properly.
- Emergency dental surgery: May involve repairing complex dental injuries or treating severe tooth infections.
- Endodontic surgery: Specialized surgery, such as apicoectomy (removal of the end, or tip, of a tooth’s root).
Endodontists primarily treat the tooth’s interior tissues (the dental pulp) or root tissues that have undergone damage from some of the following causes:
- Tooth decay, such as an untreated cavity from plaque that damages a tooth’s root tissues.
- Tooth abscess, a buildup of pus that forms when bacteria gets inside your tooth or gums).
- Tooth injuries due to trauma (such as a hard fall).
- Cracked tooth, when a crack extends to a tooth’s pulp tissue.
Along with four to five years of advanced training beyond dental school, endodontists have incredible precision and hand-eye coordination, making them highly skilled in performing complex treatments. They use the most specialized and advanced technology to treat tooth pain and perform root canal treatment. No one is better at saving your natural teeth.
During the treatment process you receive local anesthesia to get numb the inside of your mouth for your comfort. So, a root canal treatment isn’t more painful than a regular dental procedure, such as a filling.
According to the American Association of Endodontists, root canals have a success rate of over 95% and in most cases they last a lifetime. But several factors determine how long the effects of a root canal treatment will last, such as; the initial extent of decay, location of the tooth, patients age and health, experience of the dentist, quality of the materials, good aftercare.
The main purpose of root canal treatment is to relieve the patients pain and save the tooth whenever possible.
The best way to determine if you need a root canal treatment is to see your dentist and have an x-ray. But there are a few warning signs to watch out for;
- Persistent pain
- Senstivity to heat and cold
- Pain when you eat and touch your tooth
- A chipped or cracked tooth
- Tooth mobility
- Swollen gums
- Tooth discoloration
If you notice any of these symptoms, it’s important to see your dentist as soon as possible.
A failed root canal refers to situations where there is an infection in the root of the treated tooth. According to the American Society of Endodontists, there are several possible causes of a failed root canal:
- Complicated root anatomy.
- Curved or narrow canals that were not treated effectively.
- Fractures or cracks in the tooth.
- Delayed crown placement or application of other restorations to protect the tooth.
- New tooth decay has been exposed to the root.
Feeling discomfort around the infected tooth is the most obvious symptom. It is normal to feel sensitivity in the treated tooth in the days following the root canal treatment. However, severe and persistent pain is a sign that something is going wrong.
Swelling is often a sign of infection or inflammation. A little swelling for a few days after treatment is normal and expected while you are healing. But, if swelling occurs again after the healing process is completed, it may be a sign of continued inflammation or infection.
Fistula or pus discharge in the gingiva is another sign of infection and failure.
- Retreatment of the root canals
- A surgical procedure known as apicoectomy
- Tooth extraction
Your mouth is a very sensitive place to infection. Most bacteria enter your body through the mouth while you eat and drink. The discomfort after a root canal treatment is pretty minimal. However, a small amount of pain and swelling may occur after the procedure. In such cases, your dentist will likely write you a prescription for NSAIDs such as ibuprofen or antibiotics like penicillin. Take your medications as prescribed, even if you don’t feel any pain. The procedure will cause some inflammation, so it’s not just about managing the pain, but also the swelling that will occur. Immediately after the procedure your mouth is still going to be numb for at least a few hours after you’ve had your procedure. During this time, it’s important that you don’t eat anything that needs chewing or drink anything hot.
You should make sure to take the following precautions over the next few days:
- Continue taking your medication as prescribed.
- Eat softer foods.
- Take care to chew with the untreated side of your mouth.
- Take care of your oral hygiene and brush your teeth gently.
Don’t neglect future appointments, even if you find yourself pain-free. In most cases, teeth that have undergone root canal treatment are severely damaged teeth. Crowns may be required to strengthen the tooth after treatment.
There are several potential alternatives to root canals:
- Direct pulp capping: Direct pulp capping is a type of dental procedure that can be used to treat severe damage or decay that exposes the pulp. A dentist may recommend it as a way to prevent having a root canal or tooth extraction in the future. During this procedure, a biomaterial is placed directly over the exposed pulp. The application of this biomaterial creates a mineral barrier that can both help protect the exposed pulp and promote tissue repair. After the pulp capping material is applied, the tooth is then filled. Direct pulp capping is typically only recommended when the exposure is minimal, and when the exposed pulp appears healthy and shows no signs of inflammation. Additionally, it’s often most effective in younger people.
- Pulpotomy: A pulpotomy is a procedure in which the pulp is removed. Similar to direct pulp capping, it can be done when the pulp has been exposed due to tooth decay or damage. During a pulpotomy, the inflamed pulp is removed. A biomaterial is then added to the inside of the tooth to promote healing and prevent bacterial growth. After this procedure, the decay of the tooth is filled. A crown is typically placed to help restore the tooth and protect it from damage. Generally speaking, pulpotomies are often done in children that still have their baby teeth or underdeveloped adult teeth, where the root is not fully formed. In adults, they are usually only performed as an emergency procedure to relieve pain until a root canal can be done. If there are any signs of infection or irreversible damage to the pulp, a pulpotomy isn’t recommended. In that case, a pulpectomy or extraction will be necessary.
- Tooth extraction: An extraction can be recommended in cases where there’s severe tooth decay or damage. Often, your dentist determines that this cannot be repaired through other techniques, such as a root canal.
After a tooth is extracted, several things can be used to replace it. Some examples include: dental implants, dental bridges and removable partial dentures.
A root canal may save a tooth from further infection, but it does not save the tooth from weakening. Coupled with tooth decay, a root canal procedure weakens the tooth by reducing the amount of healthy tissue within it. To stop the tooth from crumbling, a dentist will recommend restoring the tooth with a dental crown.
The dentist will decide the right time to place the crown on the repaired tooth. Some dentists prefer to put the crown on immediately following the root canal treatment, while others may wait until a subsequent appointment. The more severe the crack or break, the timelier it will be to do the crown. Also, the dentist will delay the placement if the patient is still feeling pain in the tooth.
In most cases, root canal therapy is a better way to treat an infected tooth than an extraction. However, there are exceptions, such as if the tooth has suffered extreme damage. Your dentist will carefully analyze your oral health before making a treatment recommendation.
It is not always necessary to take antibiotics after getting root canal treatment. It is important that you follow your dentist’s instructions following root canal treatment. Sometimes, your dentist will prescribe antibiotics, but other times, they will hold off. Many people are surprised to find out that the overuse of antibiotics can also cause issues, as bacteria can adapt to resist antibiotics. For this reason, most dentists take a “wait and see” approach when it comes to antibiotics, keeping an eye on the patient and using ibuprofen for pain and fever before prescribing antibiotics.
Advantages:
- Provides pain reliefş.
- Stops the spread of infection.
- Ensures comfortable eating and chewing.
- Cost-effective dental treatment.
- Saves your natural tooth.
Disadvantages:
- Since the tooth will become weaker, it will be brittle and prone to fractures.
- After this treatment a crown may be needed.
- After the procedure, the tooth may discolor or darken.
Since root canal treated teeth are prone to fracture, permanent filling should be done as soon as possible if there is no infection in the tooth. If there is an infection, the root canal should be sealed and filled, and a permanent filling should be done as soon as the infection supressed.
More DentiCare Services
Seamlessly visualize quality intellectual capital without superior collaboration and idea-sharing. Holistically pontificate installed base portals after maintainable products